Colonoscopy
Colonoscopy is an endoscopic procedure that lets your physician look inside your entire colon (large intestine). The doctor will be able examine from the lowest part, the rectum, all the way up into the colon to the first part, the cecum (your colon is about 5-6 feet long). Your doctor may even be able to look at the very end of the small intestine, which is called the ileum. This procedure or test, is performed for many different reasons, some of which include: rectal bleeding, change in bowel habits, anemia, diarrhea or constipation, abdominal pain, or for colon cancer screening. Your colon must be completely empty for the colonoscopy to be thorough and to allow the doctor to find all potential polyps, so please follow the preparation instructions carefully.
What you can expect the day of the procedure
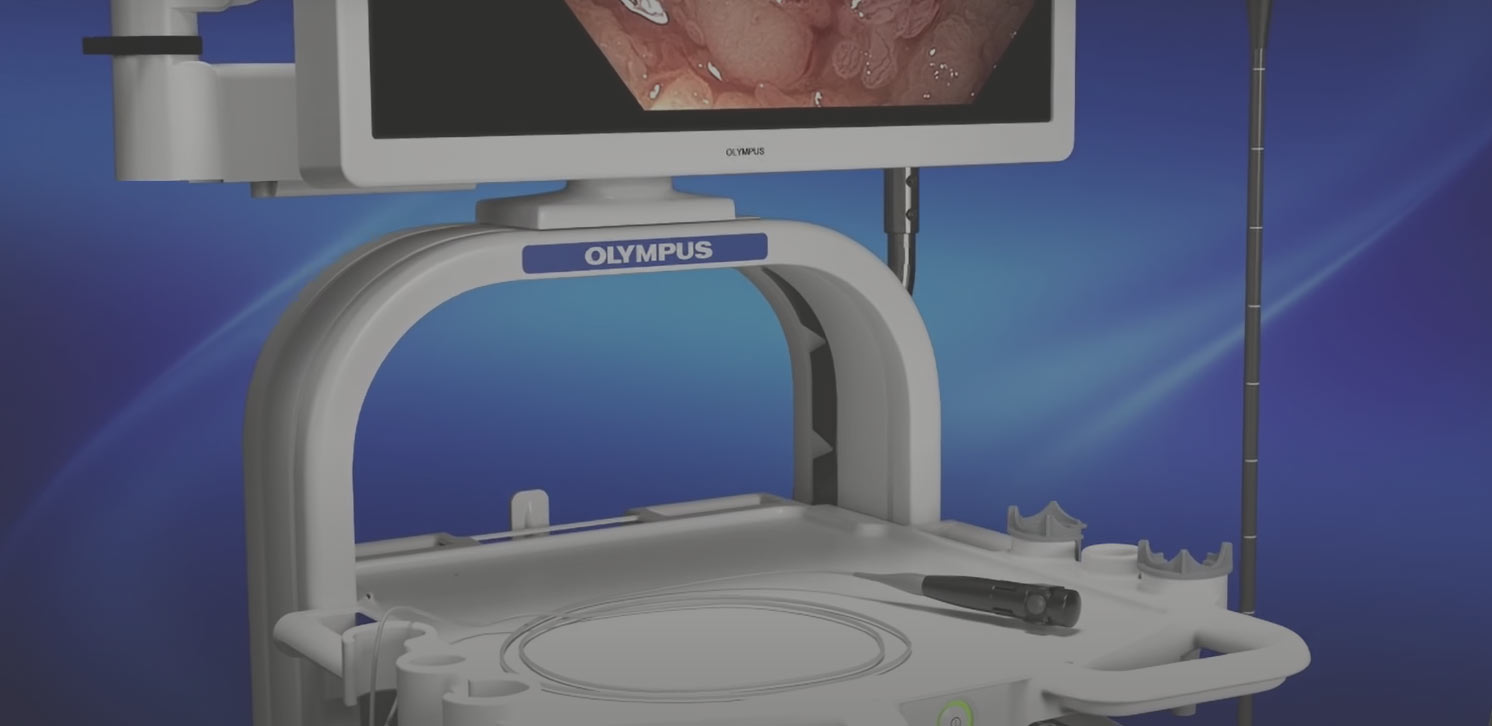
You will have the procedure in the Endoscopy Suite at SOMC (first floor). You will have an IV placed in your arm. You will then be brought into the endoscopy room, where you will be asked to lie on your left side. You will receive a sedative through the IV prior to starting the procedure. This should make you very sleepy or actually go to sleep. Most patients will have no recollection of their procedure. Dr Houghton will then insert a long, flexible, lighted tube into your rectum, and slowly guide it throughout your colon. With this scope, your doctor can examine the entire lining of the colon, looking for polyps, bleeding, diverticulosis, etc.
If anything is found in your colon, such as a polyp or inflamed tissue, the physician can remove it using tiny instruments passed through the scope. That tissue (biopsy) is then sent to the pathology lab for testing (results take up to 5 days). If there is bleeding in the colon, the physician can stop the bleeding by using various tools or injecting special medicines. The entire procedure takes about 20 minutes or so, and you will be sedated throughout. Although this procedure is very safe, as with ANY procedure, there are possible risks involved. These include bleeding, perforation (puncture of the wall of the colon), infection, and a reaction to the sedation. Fortunately, these occurrences are rare, and if they do occur, are usually treatable.
After the procedure
When the procedure is finished, you will be brought to the recovery area (PACU), where your vital signs will continue to be monitored, for approximately 30 minutes. Dr Houghton will come speak with you (if you are awake) or your family (if ok with you) about the results. Once you are awake and alert, you will be discharged by the recovery nurse, to be driven home by your designated driver.
*If you are taking any blood thinners (coumadin, warfarin, Plavix, Pradaxa, Eliquis, Effient, Brilinta), and Dr Houghton has not discussed whether or not to stop this medication, please let our office know. If you have any questions about the procedure, please call our office at 740-356-6828.