Did you know?….®
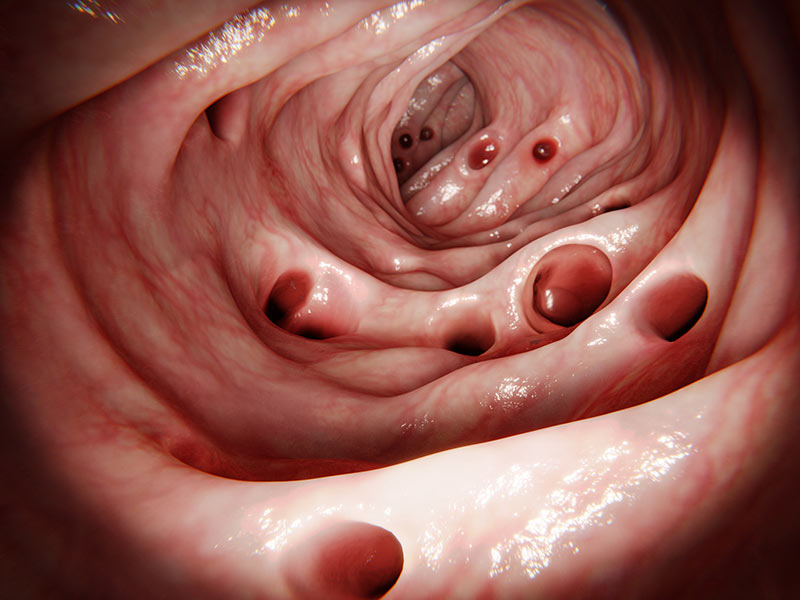
Adenoma Detection Rate (ADR), is the most important quality indicator for the colonoscopy procedure. The Adenoma Detection Rate is defined as the percentage of patients where the doctor performing a screening colonoscopy finds an adenoma (a pre-cancerous polyp). The acceptable ADR for average risk patients has been defined as at least 25%. So, if a doctor performs 100 screening colonoscopies, he or she should find pre-cancerous adenomas in at least 25 of those patients. The reason that the ADR is so important, is that it basically determines our ability to prevent colon cancer, as it is believed that all colon cancers start off as an adenoma. Studies have shown that high Adenoma Detection Rates translate into decreased rates of colon cancer. So, the higher a doctor’s ADR, the lower the chance that those patients (who had their colonoscopies) are going to develop colon cancer in their lifetime. In fact, it is believed that for every 1% increase in a doctor’s ADR, there is a 3% decrease in the risk of colon cancer!
I am very proud to report that my Adenoma Detection Rate over the past 2 years has been calculated at 51.5%. These are purely screening exams, meaning no symptoms such as rectal bleeding, change in bowel habits, constipation, etc. (I performed roughly 2,000 colonoscopies total over this time period). Thank you to Jason Martin, RN for pulling the screening colonoscopy data from our software. And to Sharon Rusnak in laboratory for pulling the pathology data.
Be well!